Introduction:
Allogeneic hematopoietic cell transplant (allo-HCT) is an effective consolidative treatment for patients with certain hematological malignancies and gives the best outcome when done in remission. However, patients with refractory acute myeloid leukemia (AML), certain forms of myeloproliferative neoplasia (MPN), and myelodysplastic syndrome (MDS) deemed unable to achieve remission with standard induction are often excluded from allo-HCT with conventional conditioning regimen as pre-transplant remission could not be achieved. Recently, a sequential transplant approach, as developed by the Munich group, comprising of intensive cytoreductive chemotherapy FLAMSA (fludarabine/amsacrine/cytarabine) to decrease leukemia cell burden shortly prior to conditioning regimen, had been successfully used for high-risk (HR) AML/MDS with promising results.
Methods:
We studied 56 patients (median age, 52 years; range 17-68) with HR AML (n=45), as defined by refractory, relapsed disease, secondary leukemia, complete remission with adverse-risk cytogenetics according to ELN criteria, or high/very high risk refined Disease Risk Index (DRI), MPN (n=2), and HR MDS (n=9) according to IPSS-R, undergoing allo-HCT using the sequential transplant approach in 2 transplant centers in Singapore between January 2009 and June 2020. The sequential transplant approach combined a cytoreductive chemotherapy, which consisted of either FLAMSA (n=17), FLAG +/- Ida [fludarabine/cytarabine/granulocyte colony stimulating factor (GCSF) +/- idarubicin] (n=23), or CLAG (clofarabine +/- cytarabine +/- GCSF) (n=15), followed by reduced intensity (RIC) (N=48) or myeloablative (MAC) (N=8) conditioning regimen. All patients received peripheral blood stem cell from matched related donors (N=30), mismatched related donors (N=3), matched unrelated donors (N=16), or mismatched unrelated donors (N=7). Post-grafting immunosuppression consisted of calcineurin inhibitor and mycophenolate mofetil in all patients. Thymoglobuline or post-transplant cyclophosphamide were added for GVHD prophylaxis in unrelated donor transplant and mismatched related donors, respectively.
Results:
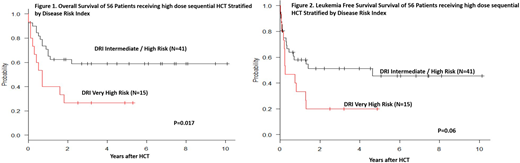
The median time to neutrophil > 1000/μL was 11 days (range, 8-19). With a median follow-up of 44 months (range, 1-123), the Kaplan-Meier estimate of overall (OS) and leukemia-free (LFS) survivals at 5 years were 49% (95% CI, 35-62) and 37% (95% CI, 23-52), respectively. The 2-years cumulative incidence of relapse and non-relapse mortality (NRM) were 47% (95% CI, 32-60) and 13% (95% CI, 6-24), respectively.
Patients receiving FLAG or CLAG-based sequential regimen showed lower cumulative incidence of NRM (2-year cumulative incidence for NRM: 5% vs 29%; p=0.018), and similar relapse (2-year cumulative incidence for relapse: 49% vs 53%; p=0.64), as compared to patients given FLAMSA-based sequential regimen, resulting in a trend towards more favourable OS (5-year OS: 53% vs 41%; p=0.29) and LFS (5-year LFS: 46% vs 20%; p=0.08). In multivariable analysis, only refined DRI showed significant impact on OS (p=0.04), but has no significant impact on LFS, NRM, and relapse. The 5-year OS for patients with intermediate/high risk and very high risk DRI were 59% and 27%, respectively (p=0.017), and the corresponding 5-year LFS were 46%, and 20% (p=0.06), respectively (Figure 1 & Figure 2). The intensity of conditioning regimen did not significantly impact on OS, LFS, relapse, and NRM.
Conclusions:
Sequential transplant conditioning with FLAMSA, FLAG or CLAG followed by allo-HCT is an effective strategy in overcoming the dismal prognosis of HR AML, MDS and MPN, and enabling favourable long-term disease-free survival. More studies on effective strategies such as post-transplant maintenance therapy with prophylactic donor lymphocyte infusion, are needed to further eliminate the risk of relapse, without increasing risk of treatment related toxicity.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal